Hypnic Jerks: How To Avoid Waking With A Jolt
 Have you ever woken up with a sudden jolt just as you were falling asleep? Maybe it felt like one arm or leg had a strong spasm?
Have you ever woken up with a sudden jolt just as you were falling asleep? Maybe it felt like one arm or leg had a strong spasm?
Perhaps you’ve even woken up feeling like you were falling, or with an unpleasant shock, loud noise or flash of light.
And it could be something your partner does at night, and their jolting movement in turn disturbs your sleep.
If any of these sound familiar, it could be that that you’ve experienced hypnic jerks.
A common occurrence
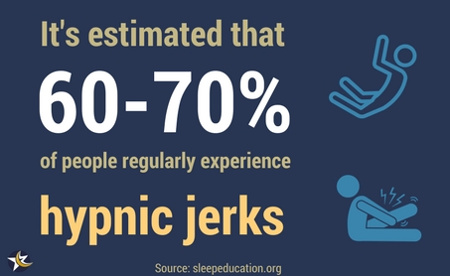
You’re certainly not alone in experiencing this strange sensation at night. It’s estimated that 60 to 70% of people experience hypnic jerks at some point in their lives.
This article will help you understand hypnic jerks better, and hopefully put your mind at ease if you’re worried about them.
You’ll also find advice for coping with them, both from professionals and previous readers.
Different names
The terminology in the world of sleep can be confusing at time. So it’s worth bearing in mind that hypnic jerks are sometimes referred to by different names:
- Sleep starts
- Night starts
- Sleep jerks
- Hypnagogic jerk
- Myoclonus, or myoclonic jerk
Symptoms
Hypnic jerks are the sudden involuntary twitching of one or more muscles when you’re falling asleep.
The latest International Classification of Sleep Disorders manual describes them as:
Sleep starts, also known as hypnic jerks, are sudden, brief, simultaneous contractions of the body or one or more body segments occurring at sleep onset. Sleep starts (or hypnic jerks) usually consist of a single contraction that often affects the body asymmetrically. The jerks may be either spontaneous or induced by stimuli.
So the fact that they usually occur asymmetrically explains why it often feels like just one arm or leg jolts.
They can occur independently, or in response to an external stimuli in the bedroom, such as your partner moving or external noise.
As well as spasms, some people might have other symptoms:
- The feeling of falling
- The sensation of pain or tingling
- Hearing a sudden noise, such as an explosion. This could also be what’s known as exploding head syndrome.
- Flashing or unusual lights
- Hallucinations
Survey results
I conducted a short survey for readers to share their experience of hypnic jerks. The results will be biased because people voting were already searching for information about the topic.
But with thousands of people participating, the results still provide some interesting insights.
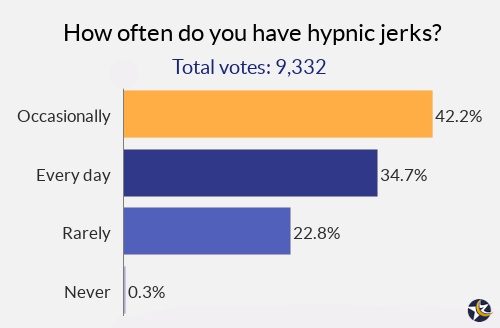
1. Frequency
In the chart below you can see how often readers experience hypnic jerks. It’s interesting to note that many people have them on a daily basis.
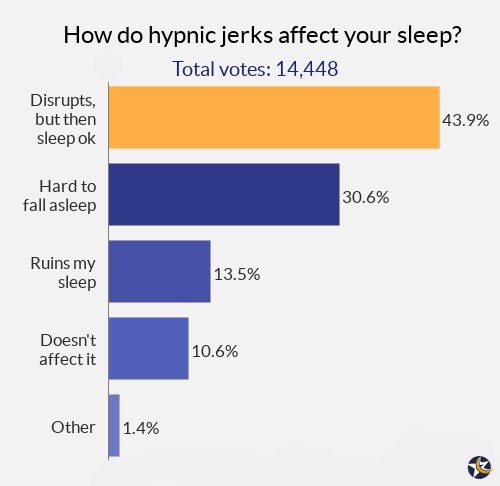
2. How they affect your sleep
An interesting point arising from question 2 is that many people are able to sleep fine even though they have them.
And that’s in line with the usual advice not to worry about them, and try to go back to sleep.
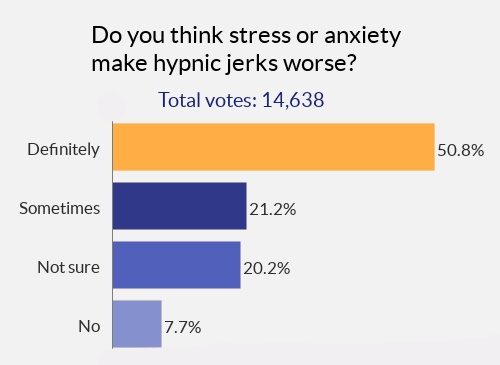
 3. The role of stress and anxiety
3. The role of stress and anxiety
The final question shows that many people feel stress or anxiety makes their hypnic jerks worse. This is also a factor which appears many times in the comments below.
So it could be that tackling stress or anxiety in your life is a good idea if it’s relevant to you.
What causes hypnic jerks?
As is often the case in the complex world of sleep, the cause still isn’t completely understood. However, there are different theories:
1. Muscles relaxing
The first theory is that they happen as your nervous system relaxes and slows down when transitioning from wakefulness to sleep. Your breathing slows down, your temperature drops and muscles relax.
A hypnic jerk might happen when nerves misfire during this slowing down process, resulting in the muscular spasm.
The International Classification of Sleep Disorders manual offers a more technical explanation:
Hypnic jerks are hypothetically caused by sudden descending volleys originating in the brainstem reticular formation activated by the system instability at the transition between wake and sleep.
2. Your brain thinks you’re falling
Another theory is that as your muscles naturally relax when falling asleep, your brain might misinterpret it as falling. So it signals to your body to tense muscles to protect you from harm.
3. Response to hallucinations or dreams
A third theory is that hypnic jerks occur in response to sleep hallucinations or the onset of dreams. This might also explain why some people have other sensations besides the physical twitching.
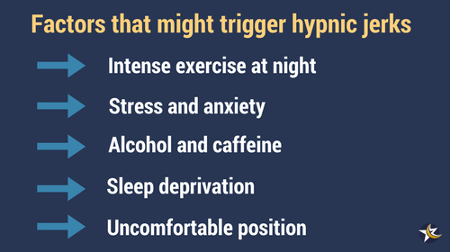
Factors that can trigger hypnic jerks
In addition to the theories above, researchers suggest factors that can lead to hypnic jerks:
- Caffeine or other stimulants
- Alcohol
- Anxiety or stress
- Heavy physical exercise late in the evening
- Sleeping in an uncomfortable position
- Being very tired or sleep deprived
Is it caused by another condition?
A study of hypnic jerks by researchers at the University of Alabama raised an important point: hypnic jerks could in some cases be a characteristic of another condition.
Some of the possibilities they suggest include:
- Noctural seizures
- Nonepileptic seizures
- Other parasomnias
- Hyperekplexia
- Restless legs syndrome
- Periodic limb movements in sleep
- Excessive fragmentary myoclonus
- Psychiatric diagnosis
In addition, researchers in Italy in 2016 found that hypnic jerks are common in people with Parkinsonism. The Alabama team also suggested it could be helpful in diagnosing the condition.
Do I need to see a doctor?
Most sleep experts advise that hypnic jerks are in most cases nothing to worry about; just relax and go back to sleep again.
However, if you have them regularly and/or severely, you might want to raise it with your primary care doctor. If they think it’s a sign of another disorder, they might ask you to do a sleep study or further tests.
And they might prescribe medication, such as clonazepam, or provide you with advice about good sleep hygiene.
How can you stop hypnic jerks?
It might not be possible to totally stop them from happening. Accepting them as normal and harmless is perhaps your best option if they aren’t severe.
In addition, the following advice might help:
- Cut down on alcohol and caffeine, especially in the evening.
- Reduce how much heavy exercise you do in the evening.
- Make sure you have enough magnesium and calcium in your diet – this can help with muscle and nerve spasms.
- Use a comfortable mattress and bedding.
- Sleep in a comfortable position.
- If you suffer from anxiety or stress, do some simple relaxation exercises in bed.
- Try not to allow yourself to get too tired. You may understandably have a busy and tiring lifestyle.But it’s important to give yourself enough time to sleep well.
Avoid the vicious cycle of worry
Hypnic jerks can trigger a vicious cycle of worry if you become fixated on them. This is a common thing that happens with many sleeping difficulties.
For example, people who have insomnia for a few nights might start worrying that they won’t be able to get to sleep. This worrying then becomes the very cause of their insomnia, even if the original cause has long gone.
If you worry about hypnic jerks, you might start to get less sleep and become more fatigued.
But both anxiety and fatigue are thought to contribute to the frequency of hypnic jerks, and so the vicious cycle begins.
The key is not to allow the occasional spasm to disrupt your sleep any more than it has to. Try to relax, forget about it and go back to sleep.
Readers’ tips for coping with hypnic jerks
In the comments below, many readers have offered suggestions for managing hypnic jerks. So I’ve compiled a list of the most common and interesting ideas.
They don’t all have medical backing, but you might find the ideas useful if nothing else has helped.
- Try to see the funny side.
- Magnesium supplements have been helpful for some readers, as has rubbing magnesium oils or transdermal magnesium into the area where you most commonly twitch. One suggestion was to get a blood test to check if you have a deficiency.
- Assess your current diet. Make sure it’s healthy and balanced. Eat less sugary and salty foods. Eat plenty of fresh fruit and vegetables.
- Don’t drink alcohol, coffee or energy drinks for a week and see if it improves.
- Don’t stress about it, as worrying makes it worse.
- Try to deal with major stress in your life.
- If you suffer from anxiety, take steps to tackle this in your daily life.
- Drink cayenne pepper tea (I suggest doing some research into this first).
- Try acupuncture.
- Make sure you get enough calcium in your normal diet, or take supplements.
- Stop doing strenuous exercise for a week and see if it improves.
- Try to see them as a sign that you must be falling asleep. So it’s a positive thing as you know you’ll soon be asleep.
- Ask your doctor if any medication you take could be causing it.
- Check if medication you’re taking has the side effects of myoclonus – a surprising amount do.
- Sleep aids and allergy medication containing the anti-histamine diphenhydramine can sometimes cause twitching.
- Sleep in a different position from your back – one suggestion was that the fetal position can help.
- Don’t go to bed late at night.
- Some people say clonazepam has helped them.
- Film yourself sleeping or use a sleep monitor. One reader said he discovered through doing this that he was snoring, and that the hypnic jerks occurred while he was snoring heavily.
- Some female readers feel that it can be connected to hormonal changes.
- Ask for a referral to a sleep clinic if it’s particularly troubling.
- Ensure you have a quiet sleeping environment. It could be a sudden noise which startles you awake.
- Stay hydrated.
- If you’re being bothered by them repeatedly, get up and do something relaxing for 10-20 minutes, then try to sleep again.
- Have a light snack before bed. And if they occur repeatedly, get up and have a light snack.
- Have a warm shower before bed. Then do relaxation exercises before getting into bed or while in bed.
- If you do exercise, it could be excess lactic acid contributing to hypnic jerks. So try looking into ways to reduce the lactic acid.
- Try apple cider vinegar. It’s used as a hiccup remedy, so might help with hypnic jerks too.
Your views
It’s always interesting to hear your experiences, and I know many readers have benefited from reading the stories and advice of others.
So please keep your comments, tips and theories coming. And if you have any practical ideas for dealing with hypnic jerks, I’ll continue to add them to the list.
Pain Management: Arachnoiditis
Arachnoiditis is a pain disorder caused by the inflammation of the arachnoid, one of the membranes that surrounds and protects the nerves of the spinal cord. It is characterized by severe stinging, burning pain, and neurological problems.
Symptoms of Arachnoiditis
Arachnoiditis has no consistent pattern of symptoms, but in many people it affects the nerves connecting to the lower back and legs. The most common symptom is pain, but arachnoiditis can also cause:
- Tingling, numbness, or weakness in the legs
- Sensations that may feel like insects crawling on the skin or water trickling down the leg
- Severe shooting pain that can be similar to an electric shock sensation
- Muscle cramps, spasms and uncontrollable twitching
- Bladder, bowel and sexual problems
As the disease progresses, symptoms may become more severe or even permanent. Many people with arachnoiditis are unable to work and suffer significant disability because they are in constant pain.
CONTINUE READING BELOW
Causes of Arachnoiditis
Inflammation of the arachnoid can lead to the formation of scar tissue and can cause the spinal nerves to stick together and malfunction. The arachnoid can become inflamed because of an irritation from one of the following sources:
- Direct injury to the spine.
- Chemicals: Dye used in myelograms (diagnostic tests in which a dye called radiographic contrast media is injected into the area surrounding the spinal cord and nerves) have been blamed for some cases of arachnoiditis. The radiographic contrast media responsible for this is no longer used, however. Also, there is concern that the preservatives found in epidural steroid injections may cause arachnoiditis.
- Infection from bacteria or viruses: Infections such as viral and fungal meningitis or tuberculosis can affect the spine.
- Chronic compression of spinal nerves: Causes for this compression include chronic degenerative disc disease or advanced spinal stenosis (narrowing of spinal column).
- Complications from spinal surgery or other invasive spinal procedures: Similar causes include multiple lumbar (lower back) punctures.
Diagnosing Arachnoiditis
Diagnosing arachnoiditis can be difficult, but tests such as the CAT scan(computerized axial tomography) or MRI (magnetic resonance imaging) have helped with diagnosis. A test called an electromyogram (EMG) can assess the severity of the ongoing damage to affected nerve roots by using electrical impulses to check nerve function.
Note: Myelograms with the radiographic contrast currently in use, combined with CAT scanning, are not considered to be responsible for causing arachnoiditis or causing it to worsen.
Treating Arachnoiditis
There is no cure for arachnoiditis. Treatment options for arachnoiditis are similar to those for other chronic painconditions. Most treatments focus on relieving pain and improving symptoms that impair daily activities. Often, health careprofessionals recommend a program of pain management, physiotherapy, exercise, and psychotherapy. Surgery for arachnoiditis is controversial, because outcomes can be poor and provide only short-term relief. Clinical trials of steroid injections and electrical stimulation are needed to determine whether those treatments are effective.

No comments:
Post a Comment